Gardasil, a risky vaccine: paradoxical cervix cancer increasing rate in vaccinated population
15 5 2019 gardasil chicago (002) 5 diaporama
Paradoxical oncologic results of Gardasil in the real world. A cancer registers study.
Dr G Delépine, surgeon oncologist, Paris, France[1] N Delépine paediatric oncologist, Paris, France[2]
Oral presentation by Dr G Delépine 24 th of may 2019 Chicago Illinois USA
Summary
Aim: the authors evaluate the results of HPV vaccination on the incidence of invasive cervical cancer in different countries, comparing published data in national cancer registries and those of HPV vaccine coverage.
Method. After collecting crude figures and standardized incidences from oncologic registers of Australia (Australian Institute of Health and Welfare), Great Britain (Cancer research UK), Sweden and Norway (Nordcan), they analyse the evolution and their tendencies before and after the era of vaccination in the different countries and different age groups, with a particular attention to 20-29 age groups(high vaccine coverage).
Results In all studied countries, these evolutions are similar. During the 1989-2007 ( pre-anti HPV vaccination period), the incidence of invasive cervical cancer declined in all countries, results linked with smear screening.
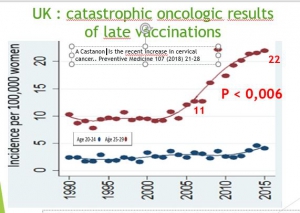
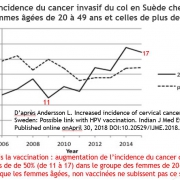
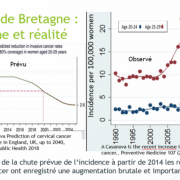
Vaccination campaigns were initiated in 2007 (Australia) or 2008 (Great Britain), and we have now 7 to 9 years of follow up. Since 2007, a trend reversal has been observed in all countries with high immunization coverage studied (Australia, Great Britain, Norway, Sweden). Their official cancer registries reveal an increase in the incidence of invasive cervical cancer that appears 3 to 5 years after the beginning of the vaccination campaign and affects almost exclusively the age groups the most vaccinated.
In 20-24 group the increase reaches 100% in Sweden (1.86/100000 in 2007 vs 3.72 in 2015), 70% in Great Britain, (2,7 in 2007 vs 4,6 in 2014), 113% in Australia (0.7 vs 1.5), 10% in Norway (2.18 in 2007 vs 2.4 in 2015). In the 25-29 age groups, the increase reaches 100% in Great Britain (11 in 2007 vs 22 in 2016), 36% in Australia (5.9 in 2007 vs 8 in 2014), 9% in Norway (5.9 in 2007 vs 8 in 2015),10% in Sweden.
The crude figures are small, and, for this reason, the differences are individually not all statistically significant, but their convergence constitute a strong alarm signal, while unvaccinated (older women) have their risk of cervical cancer stabilized or continuing to decrease.
Comments. The contrast of the increasing rate of invasive cancer despite nearly eradication of HPV viruses after vaccination is paradoxical.
For vaccinated women, the evolution is dramatic. In France, a country with low vaccination coverage (<20%), the world standardized incidence rate of cervical cancer continues to decline in all age groups and is now lower (2017ASR 6/100000) than of more vaccinated countries
Conclusion. This unexpected paradoxical result, absolutely distressing for vaccinated women, requires additional studies to determine as quickly as possible the causes of such a health disaster and justifies an immediate review of vaccine recommendations.
[1] No link of financial interest with any drug company or anti-vaccine association
[2] Idem 1